The electroconvulsive therapy , formerly known as electroshock therapy, is a psychiatric treatment in which seizures are electrically induced in patients to provide relief from the disorders mental. The procedure was first performed in 1938 and is the only form currently used in psychiatry. It is often used with informed consent as the last line of intervention for major depressive disorder, mania, and catatonia.
It is a modern, safe and effective therapy, as it can alleviate the symptoms of the most serious forms of depression more effectively than medication, but because it is an intrusive procedure and can cause some memory problems , it should be used only when absolutely necessary.
Index
What is the medical use of electroconvulsive therapy?
It is used with informed consent and in conditions where there is a need for a rapid and definitive response due to the severity of a psychiatric disorder or medical condition (for example, when the illness is characterized by stupor, marked psychomotor retardation, depressive delusions, hallucinations, or life-threatening physical exhaustion associated with mania).
Major depressive disorder
For major depressive disorder , electroconvulsive therapy is generally used only when other treatments have failed, or in emergencies, such as impending suicide , it has also been used in selected cases of depression that occurs in the setting of multiple sclerosis, the disease of Parkinson’s , Huntington’s disease , developmental delay, cerebral arteriovenous malformations, and hydrocephalus.
Catatonia
Electroconvulsive therapy is generally a second-line treatment for people with catatonia who do not respond to other treatments, but only for severe or life-threatening catatonia. There is a lack of clinical evidence of its efficacy but excellent efficacy in catatonia is generally recognized. For people with autism spectrum disorders who have catatonia, there is little published evidence on efficacy.
Mania
This type of therapy is used to treat people who have severe or prolonged mania, it is recommended only in life-threatening situations or when other treatments have failed, and as a second-line treatment for bipolar mania.
Schizophrenia
Electroconvulsive therapy is rarely used in refractory schizophrenia , but is sometimes recommended when short-term overall improvement is desired, or the subject shows little response to antipsychotics alone. It is useful in the case of severe exacerbations of catatonic schizophrenia .
What are bilateral and unilateral electroconvulsive therapies? – Techniques.
When we refer to bilateral, the electrical current passes through the entire brain. And when one-sided reference is made, the current has just passed through one side and both of them cause a seizure throughout the brain.
Bilateral electroconvulsive therapy appears to work faster and more efficiently and is probably the most widely used in Great Britain; however, there are concerns that it may cause more side effects.
The unilateral is now used less, it was thought to cause less memory loss, but recent research has shown that it is necessary to use higher doses of electricity to be as effective as the bilateral. If the dose of electricity is increased to be equally effective, the risks of memory loss are as great as with bilateral.
Sometimes electroconvulsive therapy clinics will start a treatment cycle with bilateral and switch to unilateral if the patient experiences side effects. Alternatively, they can start with unilateral and switch to bilateral if the person does not improve. You may want to talk to your doctor about which of the two is best for you.
What happens during electroconvulsive therapy? – Procedure.
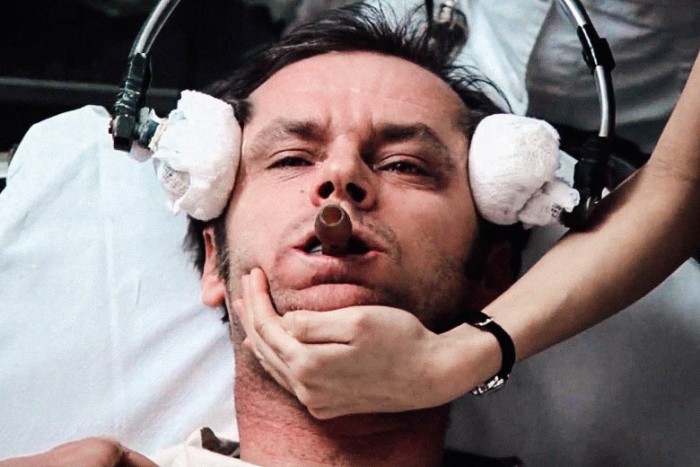
Treatment is usually given in the morning, before breakfast. Before the actual treatment the person is given general anesthesia and a muscle relaxant. The electrodes are placed on one side (unilateral) or both (bilateral) of the scalp and a small electrical current is passed between them until a brief generalized seizure occurs, the person feels nothing due to the anesthesia and does not convulse due to the relaxant muscular.
You wake up five to 10 minutes after treatment and usually have a clear head within 30 minutes. Often they do not clearly remember the time elapsed around the treatment and may at first have little memory about the period of illness surrounding the treatment, the memory of these events gradually returns.
If electroconvulsive therapy is done on an outpatient basis, a family member or friend should drive the person home after the procedure (no driving is allowed for 24 hours after a session) and stay until they go to sleep that night.
Treatments are generally given two to three times a week for three to six weeks, although the exact course depends on the nature of the disease and the person’s response to treatment, it should be reassessed after each session.
In general, symptoms start to improve after two sessions. Treatment should be stopped as soon as the person has responded appropriately, if there are adverse effects or if consent is withdrawn. Exactly how electroconvulsive therapy works to treat depression is not understood, and results can vary from person to person.
How often is electroconvulsive therapy given?
Most units administer it twice a week, it is impossible to predict how many treatments someone will need. However, in general, it will take 2-3 treatments before you see any difference, and 4-5 treatments for noticeable improvement.
A course will be, on average, 6 to 8 treatments, although up to 12 may be needed, especially if you have been depressed for a long time, if after 12 treatments, you do not feel better, electroconvulsive therapy is unlikely to help and the course it will usually be discontinued. A member of the mental health team should check after each treatment to see how you are responding and to check for troublesome side effects. Your consultant should see you after every other treatment and should stop as soon as you have made a recovery or if you say you no longer want to have it.
Effects of Electroconvulsive Therapy
In addition to the effects on the brain, the general physical risks are similar to those of brief general anesthesia. Immediately after treatment, the most common adverse effects are confusion and memory loss and therefore it should be used with great caution in people with epilepsy or other neurological disorders because, by its nature, it causes small tonic-clonic attacks, so it probably not it is given to a person whose epilepsy is not well controlled.
Some patients experience muscle pain, this is due to muscle relaxants given during the procedure and rarely due to muscle activity and if combined with deep sleep therapy it can lead to brain damage if given in a way that leads to hypoxia or anoxia in the patient.
In memory of
The retrograde amnesia occurs to some extent in almost all recipients of electroconvulsive therapy. The American Psychiatric Association report (2001) acknowledges: “In some patients, recovery from retrograde amnesia will be incomplete, and evidence has shown that it can cause persistent or permanent memory loss.” It is the supposed effects on long-term memory that generate great concern about its use. However, the methods used to measure memory loss are generally poor, and their application to people with depression, who have cognitive deficits including memory problems, has been problematic.
Acute effects can include amnesia, both retrograde (for events that occur before treatment) and anterograde (for events that occur after treatment). Memory loss and confusion are more pronounced with bilateral rather than unilateral electrode placement, and with an outdated sine wave rather than brief pulse currents.
In the structure of the brain
There is considerable controversy about the effects on brain tissue, although several mental health associations, including the American Psychiatric Association, have concluded that there is no evidence that electroconvulsive therapy causes structural brain damage.
In pregnancy
If steps are taken to lessen the potential risks, it is generally accepted that this therapy is relatively safe during all trimesters of pregnancy, particularly when compared to drug treatments. Suggested preparation for electroconvulsive therapy during pregnancy includes a pelvic examination, discontinuation of nonessential anticholinergic medication, uterine tocodynamics, intravenous hydration, and administration of a non-particulate antacid.
During therapy, elevation of the pregnant woman’s right hip, external fetal cardiac monitoring, intubation, and prevention of excessive hyperventilation are recommended. In many cases of active mood disorder, the risks of untreated symptoms may outweigh the risks. Possible complications can be minimized by modifications in technique, use during pregnancy requires a thorough evaluation of the patient’s capacity for informed consent.
Is Electroconvulsive Therapy a Good Option?
The patient and the doctor must analyze all the available options before deciding on any treatment, if this type of therapy is recommended, the patient must receive a complete medical examination that includes a history, a physical, neurological examination, electrocardiogram and a test of laboratory. Medications need to be closely watched and controlled, as do heart conditions and hypertension. The patient and family should be educated and informed about the procedure through videos, written material, discussion and any other available means before signing a written consent.
The procedure must be administered by trained healthcare professionals with experience in administering electroconvulsive therapy, as well as by an anesthesiologist specifically trained and certified to administer anesthesia. The seizure initiated by the electrical stimulus varies from person to person and must be carefully monitored by the administration team and must be performed using an electroencephalogram technique.
Nature, its history of abuse, unfavorable medical and media reports, and testimony from former patients all contribute to the debate surrounding its use. Research must continue and techniques must be refined to maximize efficacy and minimize the risks and side effects that result from such therapy.
Hello, how are you? My name is Georgia Tarrant, and I am a clinical psychologist. In everyday life, professional obligations seem to predominate over our personal life. It's as if work takes up more and more of the time we'd love to devote to our love life, our family, or even a moment of leisure.